- Cardiogenic shock happens when the heart suddenly can’t pump enough blood, causing severe drops in oxygen and rapid worsening of symptoms.
- Diagnosis typically involves ECG, echocardiogram, blood tests, and imaging to identify the underlying cause and guide urgent treatment.
- Treatment may include medications, catheterization, ECMO, surgery, or heart transplant, depending on the severity and response to care.
Cardiogenic shock is a life-threatening condition in which the heart can’t pump enough blood to meet the body’s needs. This leads to a serious drop in oxygen delivery to tissues and triggers symptoms like rapid breathing, sudden fainting, and a fast heart rate. Understanding these early signs can help ensure urgent medical care.
This condition most often happens after a heart attack but can also result from cardiomyopathies, myocarditis, or acute mitral regurgitation. Because cardiogenic shock progresses quickly, it requires immediate hospital evaluation to confirm the diagnosis and begin treatment. Prompt care is essential to prevent organ failure or death.
Many treatments can help stabilize the heart and restore blood flow, including medications, catheter-based procedures, ECMO, surgery, or even heart transplantation. The best approach depends on the underlying cause and how severely the heart has been affected.
Main symptoms
The main symptoms of cardiogenic shock include:
-
Chest pain or pressure
-
Rapid breathing or severe shortness of breath
-
Markedly increased heart rate
-
Weak pulse
-
Pale, cold, moist, or clammy skin
-
Decreased urine output
-
Altered consciousness or fainting
Cardiogenic shock may also cause fluid buildup in the lungs (pulmonary edema), which can result in shortness of breath and abnormal breathing sounds, such as wheezing.
If cardiogenic shock is suspected, urgent evaluation at a hospital is critical.
Confirming a diagnosis
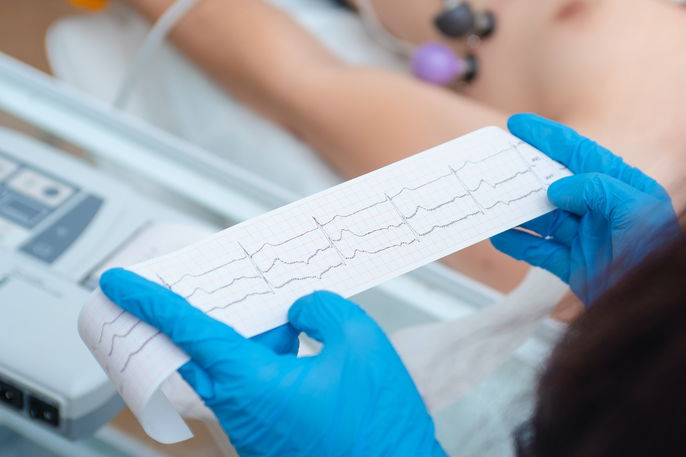
A cardiologist diagnoses cardiogenic shock in the hospital by evaluating symptoms, reviewing medical history, checking blood pressure, and performing physical, laboratory, and imaging exams.
Common tests include an electrocardiogram, echocardiogram, chest X-ray, or coronary angiography. Blood tests, cardiac enzyme measurements, and arterial blood gases may also be ordered to confirm the diagnosis and determine the most appropriate treatment.
Possible causes
The main causes of cardiogenic shock are:
-
Heart attack
-
Myocarditis or endocarditis
-
Acute mitral regurgitation
-
Cardiac arrhythmias, cardiomyopathies, or heart failure
-
Direct trauma to the heart
-
Cardiac tamponade or pulmonary embolism
-
Medication or illicit drug overdose or intoxication
In advanced cases of sepsis, a widespread severe infection, septic shock can occur and lead to cardiac involvement. This may progress to cardiogenic shock, which is associated with a very high risk of death.
Also recommended: Septicemia: Symptoms, Diagnosis, Causes & Treatment tuasaude.com/en/septicemiaTreatment options
Treatment for cardiogenic shock must be performed in the hospital by a cardiologist to relieve symptoms, support the heart’s function, and improve blood flow.
1. Use of medications
In addition to IV fluids used to maintain hydration and nutrition, the doctor may administer:
-
Vasopressors such as epinephrine, norepinephrine, or dopamine to treat low blood pressure
-
Inotropic agents such as dobutamine, dopamine, or milrinone to help the heart pump more effectively
-
Antiplatelet drugs such as aspirin, clopidogrel, or tirofiban to prevent blood clot formation
-
Anticoagulants such as heparin to reduce blood clotting and prevent new clots
-
Diuretics such as furosemide or spironolactone to reduce fluid buildup in the lungs
Many of these medications are administered intravenously for at least the first week of treatment and may later be switched to oral forms as the condition improves.
2. Catheterization
Cardiac catheterization may be performed to restore blood flow to the heart when cardiogenic shock is caused by a heart attack. A thin catheter is inserted through an artery, usually in the groin or arm, and guided to the heart to remove a clot and reopen blood flow.
3. ECMO
Extracorporeal membrane oxygenation (ECMO) acts as an external artificial lung. It helps improve blood flow and oxygen delivery to the body while cardiogenic shock is being treated.
4. Surgery
Surgery is typically recommended only in severe cases or when medications and catheter-based treatments are not effective. It may be used to repair a heart injury or to perform coronary bypass surgery, in which another artery is placed to reroute blood flow around a blocked area.
5. Heart transplant
When heart function is severely impaired and no other treatment is effective, a heart transplant may be considered. However, finding a compatible donor can be challenging and may delay the procedure.
Possible complications
Complications of cardiogenic shock include failure of multiple organs such as the kidneys, brain, and liver. This condition accounts for many deaths in intensive care units. Early diagnosis and treatment significantly reduce the risk of complications.






























